Abstract
Thrombotic and thromboembolic complications in patients diagnosed with coronavirus disease 2019 (COVID-19) are emerging as important sequelae that contribute to mortality, including disseminated intravascular coagulation, pulmonary embolism, deep vein thrombosis, ischemic stroke, and myocardial infraction. Reported incidence of thrombotic and thromboembolic complications in moderate/severe COVID-19 patients is from 21% to 49%, while even higher incidence in non-surviving COVID-19 patients. However, the underlying mechanism between thrombosis and COVID-19 is still unclear.
Tissue-type plasminogen activator (tPA) plays an important role on initiating fibrinolysis by converting zymogen plasminogen to plasmin, a serine protease that degrades the fibrin clot, and therefore preventing excessive pathological blood clots. A homologous protein to plasminogen is apolipoprotein(a) [apo(a)], a major component of lipoprotein(a). The apo(a) inhibits fibrinolysis and exacerbates thrombosis through blocking the conversion from Glu-plasminogen to Lys-plasminogen, which has a higher binding affinity to fibrin and is a better substrate to tPA. The population distribution of plasma apo(a) level is positively skewed (most values are clustered around the left tail of the distribution close to zero), and the plasma apo(a) level in most people is less than 300 μg/mL. High plasma concentration of apo(a) (> 300 μg/mL), or genetic variants of LPA, the gene that encodes for apo(a), correlates with thrombotic cardiovascular risk and thromboembolic risk in many population-based clinical or genetic studies. To investigate the potential correlation between infection of SARS-COV-2 and thrombosis, we tested de-identified plasma samples collected from hospitalized patients with or without positivity of SARS-CoV-2 testing results and COVID-19 diagnosis (ICD10CM:U07.1) through the COVD-19 Tissue Bank at the Medical College of Wisconsin. The tPA enzymatic activity was measured by the release of p-nitroaniline chromophore from a plasmin-specific synthetic substrate with exogenous human plasminogen, with the intensity of color proportional to tPA activity. The apo(a) concentration is measured by ELISA capturing total apo(a) antigen.
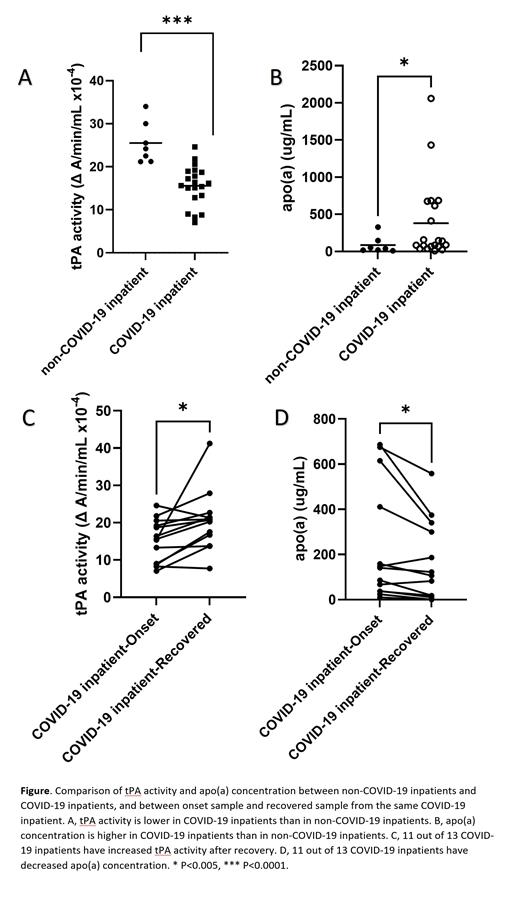
Our results show that the SARS-CoV-2-positive inpatients have higher plasma tPA concentration than the SARS-CoV-2 negative inpatients (6.0 versus 3.0 ng/mL, p<0.05), while plasma tPA enzymatic activity is lower in SARS-CoV-2-positive inpatients than the SARS-CoV-2 negative inpatients (15.2 versus 25.5 ΔA/min/mL/10 4, p<0.0001) (Figure A). The plasma apo(a) concentration is significantly higher in SARS-CoV-2-positive inpatients than in the plasma from SARS-CoV-2-negative inpatients (the median of the two groups are 114.8 versus 34.4 μg/mL, p<0.05) (Figure B). Among the 20 hospitalized patients with COVID-19, 13 survived. The 13 survived patients have one additional plasma sample collected after recovering from COVID-19 (date range between the two blood collections of onset and after recovery is from 19 to 87 days, the mean duration is 42 days). After recovery, 11 out of 13 surviving patients have increased plasma tPA enzymatic activity (the mean value at onset versus recovery is 5.2 versus 7.1 ΔA/min/mL/10 4, p<0.05) (Figure C). Consistently, 11 out of 13 surviving patients have decreased plasma apo(a) concentration compared to the plasma collected during the onset of COVID-19 from the same individuals (the median values of the onset and recovery are 141.1 versus 106.5 μg/mL, p<0.001) (Figure D).
In summary, our study shows lower tPA enzymatic activity and higher apo(a) concentration in SARS-CoV-2-positive hospitalized patients compared to SARS-CoV-2-negative hospitalized patients. Among the survived patients, the reduction of apo(a) concentration after recovering from COVID-19 is accordance with the increase of tPA enzymatic activity. Considering the role of apo(a) in inhibiting fibrinolysis through limiting tPA-mediated plasminogen to plasmin conversion, the alteration in apo(a) concentration provide a possible explanation of change of tPA activity in patients with severe COVID-19.
Baumann Kreuziger: CSL Behring: Consultancy; Quercegen Pharmaceuticals: Consultancy; Vaccine Injury Compensation Program: Consultancy.